| This is a document in a five-part series on blood cells and anemia: |
| 1. Blood cells and the CBC |
| 2. Anemia: Pathophysiologic Consequences, Classification, and Clinical Investigation |
| 3. Nutritional Anemias and Anemia of Chronic Disease |
| 4. Hemolytic Anemias |
| 5. Hemoglobinopathies and Thalassemias |
I. Introduction and definitions
Previously we have looked at nutritional anemias and the anemia of chronic disease, in which the metabolic needs of erythrocyte development are not met. The result is failure to produce enough healthy red cells. Now we turn to conditions in which the erythrocyte construction industry is healthy, but where the red cells produced are incapable of surviving the normal 120-day life span. These hemolytic anemias may be due to either intrinsic defects in rbc structure/function or a hostile external environment in which the cells are forced to live. To start with a few definitions:
- Hemolysis: Any condition characterized by a significantly decreased erythrocyte life span.
- Compensated hemolytic state: A state of hemolysis in which the resulting increased erythrocyte production is able to keep up with accelerated rbc destruction, thus averting any anemia.
- Hemolytic anemia: A state of hemolysis in which increased erythrocyte production is insufficient to keep up with accelerated rbc destruction, thus producing anemia. This anemia is characterized as normochromic/normocytic, except when sufficient outpouring of the larger reticulocytes produces a resulting elevation of the MCV.
II. Diagnosis of hemolytic anemia
Diagnosis of hemolytic anemia is performed in four steps:
- Establish that anemia exists.The diagnosis of anemia has been previously covered.
- Look for marrow responseThe sine qua non for the diagnosis of hemolysis is demonstration of an attempted marrow response to erythrocyte destruction. The classic way to do this is with the reticulocyte count. Remember that you must correct the count for the degree of anemia to prevent overdiagnosis of hemolysis. The absolute retic count (in cells/µL) or, better, the reticulocyte production index (RPI) can be used to avoid this pitfall. Even so, one should never take a positive result out of context . A classic cause of reticulosis is recovery from a nutritional anemia (esp. iron and folate). For this reason, you also need corroborating evidence of erythrocyte destruction, thus:
- Look for erythrocyte detritusWe have previously discussed the fate of destroyed red cells and their component catabolites, such as free hemoglobin, methemoglobin, methemalbumin, bilirubin, and urobilinogen, as well as the specific binding proteins for these catabolites, such as haptoglobin and hemopexin. Laboratory measurement of some or all of these assists in the diagnosis of hemolysis.
- Establish the pathophysiological mechanism of hemolysisThe first distinction to make is to determine whether the hemolysis is taking place in the sinusoids of the reticuloendothelial system (extravascular hemolysis) or in the bloodstream proper (intravascular hemolysis). Both types produce indirect hyperbilirubinemia, urobilinogen in stool and urine, decreased serum haptoglobin, and reticulocytosis. In addition, assuming hemolysis is brisk enough to overwhelm the haptoglobin hemoglobin salvage mechanism, intravascular hemolysis produces hemosiderin in the urine sediment, free hemoglobin in the serum (which may be grossly visible), and free denatured hemoglobin in the urine. Some intravascular hemolytic conditions due to mechanical destruction of rbc’s produce the helmet-shapedschizocytes (or “schistocytes”), which can be seen on the routine peripheral blood film. Extravascular hemolytic anemias may produce spherocytes, which are the result of an rbc having a narrow escape from the clutches of the RES.
The next determination to make is the mechanism of rbc destruction. Performing a thorough history and physical (including family and drug history), examining the peripheral blood film, and ordering a few inexpensive laboratory tests, such as the direct antiglobulin (Coombs’) test for autoantibodies directed against the rbc membrane antigens and the hemoglobin electrophoresis, will lead you into Diagnosisland in 95+% of the cases. Rare cases will require labor-intensive, costly tests that have to be sent away somewhere like King of Prussia, Pennsylvania, or that are batched for six months in a dusty, coffee-stained research lab tucked away in a closet into which the Medicare inspector has yet to stumble.
III. Specific Conditions
Let us consider selected hemolytic anemias individually. These particular diseases are covered either because they are common or because they illustrate important pathophysiologic features (or both).
A. Mechanical hemolytic anemias
These are certainly the easiest to understand, even to the most concrete of thinkers. Red cells are destroyed due to hydrodynamic turbulence when they are forced over gross obstructions (such as an artificial heart valve) or “clotheslined” by innumerable fibrin strands in such microangiopathic conditions as disseminated intravascular coagulation (better known by the machonym “DIC,” covered later in the heme bloc) or thrombotic thrombocytopenic purpura (TTP), an uncommon and mysterious disease of unknown etiology. The hallmark of microangiopathic hemolytic anemia is the presence of schizocytes on the routine blood film.
| Schizocytes |
|---|
 |
B. Immunohemolytic anemias
In autoimmune hemolytic anemias, the body discourteously mounts an immune attack against its own rbc membrane antigens. This condition not surprisingly tends to occur in states characterized by systemic autoimmunity, such as lupus erythematosus. If the autoantibody is of the IgG class, hemolysis will usually occur at any temperature ( “warm autoimmune hemolytic anemia” ). Several drugs are known to produce warm autoimmune hemolytic anemia which goes away after withdrawal of the drug. Typically the antibody in warm hemolysis is one directed against a universal component of the Rh system absent only in individuals (usually of native Australian blood) with the extremely rare Rh-null rbc membrane phenotype
Autoantibodies of the IgM class typically produce cold agglutinin syndrome, in which the patient is at greater risk of symptoms in a low-temperature environment. Cold agglutinin syndrome may occasionally occur transiently in cases of Mycoplasma pneumonia and rarely infectious mononucleosis. Most cold autoagglutinins are directed against the I antigen, found in almost all adults. The rare infectious mono cold agglutinin has been characterized as anti-i.
Paroxysmal cold hemoglobinuria is a very rare syndrome in which intravascular hemolysis is produced upon exposure to cold temperature by an IgG autoantibody directed against the P antigen found on the red cells of nearly all individuals.
In alloimmune hemolytic anemia, the body synthesizes antibodies against red cell antigens foreign to the host. These antibodies may be naturally occurring (such as those directed against ABO blood group antigens) or acquired as a result of blood transfusion (including that from a fetus to its pregnant mother). Acquired antibodies include those directed against the Rh, Kell, Duffy, and Kidd system antigens. Clinical hemolysis occurs 1) when maternal antibodies send a raiding party across the placenta to raise a little hell in Fetusville (to produce hemolytic disease of the newborn „ “erythroblastosis fetalis”), and 2) when host antibodies destroy transfused red blood cells in a hemolytic transfusion reaction (which fortunately is very rare with modern blood banking practices).
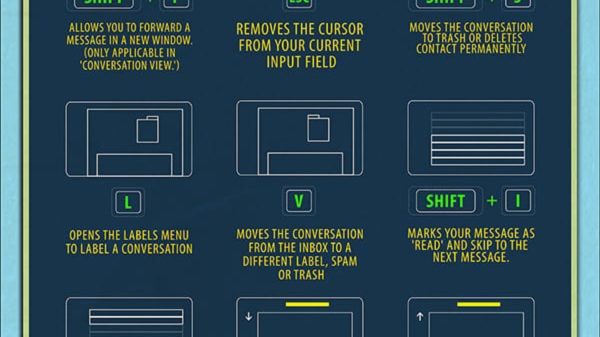
Diagnosis of immunohemolytic anemia is made by demonstrating (after having proved hemolysis is occurring, as discussed above) a positive result on a simple agglutination test to demonstrate that antibodies are present on the surface of the patient’s rbc’s. This test is properly called the direct antiglobulin test. All but the most pedantic eschew this term, preferring the eponymous designation direct Coombs’ test. Another term for immunohemolytic anemia is, therefore, “Coombs’-positive hemolytic anemia.” The diagram below illustrates the principle of the Coombs’ test:

Treatment of immunohemolytic anemias is aimed at reducing the activity of the body’s misdirected immune system. Glucocorticoids are the mainstay of therapy, although refractory cases can be treated with other immunosuppressive drugs and by splenectomy. This latter may be of benefit since immunohemolytic anemias most commonly are due to extravascular destruction of the auto-opsonized cells, at least some of which may occur in the spleen. Transfusion is of limited or no benefit (unless you can find a few Australian aboriginal blood donors), since the patient’s autoantibodies very willingly go to work on the transfused red cells with as much relish as they do on the patient’s own.
C. Paroxysmal nocturnal hemoglobinuria
This is sort of analogous to the Holy Roman Empire in that PNH is often neither paroxysmal, nor nocturnal, nor productive of gross hemoglobinuria. What does happen is that the patient’s rbcs develop an acquired somatic mutation that affects the structure of the cell membrane and makes it more sensitive to nonspecific attachment and activation of complement (sounds pretty vague doesn’t it? At least there’s no complicated mechanism to memorize). Intravascular hemolysis is the result, producing anemia if not always hemoglobinuria. In such cases of suspected chronic intravascular hemolysis without a positive urine hemoglobin test, a good thing to try is staining the urine sediment with Prussian blue reagent; the hemosiderinuria thus detected will lead you to the correct diagnosis.
D. Glucose-6-phosphate dehydrogenase deficiency
The vicissitudes of life as a red cell include the potential for harm brought about by the accumulation, through natural metabolic activities, of hydrogen peroxide (H2O2). Accumulation of peroxide is especially pronounced in exposure to certain “oxidative” substances in foods (such as fava beans) and the pharmacopìia (such as sulfonamide antimicrobials, nalidixic acid [NeGram], a urinary tract antimicrobial quinolone], nitrofurantoin [Furadantin, another UTI drug], and certain antimalarials). Fortunately, the cell has means by which peroxide can be turned into harmless water, as illustrated on the next page. The enzyme which is responsible for reduction of the peroxide to water is glutathione peroxidase. It relies on a supply of reduced glutathione to act as a reducing agent. The exhausted, oxidized glutathione must be reduced by NADPH, the only source of which is the first step in the ever-hated-by-med-students-suffering-through-biochemistry hexose monophosphate shunt (a.k.a., pentose phosphate pathway). The enzyme that presides over this first step is glucose-6-phosphate dehydrogenase. In an X-linked recessive genetic variant, the activity of G-6-PD is depressed, so that exposure to the oxidative substances overwhelms the weakened compensatory mechanism, and hemolysis, often severe and intravascular, results. Obviously, the vast majority of these patients are males (since it is X-linked). Unlike sickle cell disease, the condition may be present from birth, although there is great variation in the clinical severity of the various mutations. For instance, the G-6-PD deficiency found in eleven per cent of African-Americans is usually subclinical throughout the life of the patient, while some variants seen in Mediterranean Caucasians may be catastrophic at birth. The incidence of G-6-PD deficiency of one type or another varies from 0.1% in Germanic/Slavic/Baltic types to 50% in Kurdish Jews.

E. Pyruvate kinase deficiency
Since the erythrocyte has no mitochondria, it has no Krebs cycle. Its only source of ATP is through the Embden-Myerhof pathway (the hexose monophosphate shunt does not generate any high-energy phosphate bonds, thus no ATP). ATP is needed primarily for the maintenance of the ATP-dependent potassium/sodium pump (see illustration).

The pump is necessary to keep potassium in the cell and sodium out. If this does not happen, everything goes haywire and the cell lyses. Since this pump activity flies in the face of entropy, energy must be added to the system. As you might expect in a publish-or-perish academic system, someone has described genetic deficiencies of just about all of the Embden-Myerhof pathway enzymes. Fortunately for medical students in a memorize-or-perish academic system, the only one ever found on the National Boards is pyruvate kinase deficiency. All of the others are extraordinarily rare. PK deficiency differs somewhat from G-6-PD deficiency. The mode of inheritance is autosomal recessive. Also, the hemolysis is chronic and ongoing, unlike G-6-PD deficiency, which characteristically is episodic and related to environmental exposures, as noted above.
F. Spherocytosis
Spherocytes are seen in a variety of hemolytic anemias, specifically those in which the RES is involved in removing the cells. Examples would be immunohemolytic anemias (see above) and hypersplenism (see below). In such cases the spherocytosis is asecondary change due to escape and repair of a partially damaged rbc’s from the RES.
| Spherocytes |
|---|
 |
In hereditary spherocytosis (HS), on the other hand, a genetic variant of the structure of a cytoskeletal protein (probably spectrin, whatever that is) results in the marrow producing spherocytes de novo. These rotund cells are your basic spleen-fodder, and extravascular hemolysis is the result. The mutation is inherited as an autosomal dominant. The diagnosis is made by the use of the osmotic fragility test, in which it is demonstrated that spherocytes are more fragile when placed in a hypo-osmotic environment than are normal rbc’s. Also, it is necessary to demonstrate a negative direct Coombs’ test to rule out immunohemolytic anemia. An interesting feature of hereditary spherocytosis seen almost nowhere else is increase in the MCHC. Spherocytes may be easy to see on the peripheral smear of some patients, but in others the abnormality is so subtle, that HS cannot be ruled out based on normal RBC morphology.
Hereditary spherocytosis can be cured by splenectomy, making HS one of the very few curable hematologic conditions, and one of the only three (with some iron-deficiency anemias and a few cases of megaloblastic anemia) that can be cured by surgery.
G. Hypersplenism
Any condition which causes enlargement of the spleen turns it into a labyrinth of horrors for even the most normal corn-fed, Oklahoma-bred, antibody-free, enzyme-stuffed, glutathione-replete erythrocyte. Thus even normal rbcs can undergo hemolysis when sufficiently jacked around with. The condition is termed, somewhat vaguely, hypersplenism. You should think of this when a patient with chronic liver disease, leukemia/lymphoma, and congestive heart failure (all of which may produce splenomegaly) turns up with a hemolytic anemia and a negative direct Coombs’ test.
H. Infections of the RBC
In some infections, hemolysis dominates the clinical picture. Malaria, Carrión’s disease, and babesiosis are covered elsewhere. Clostridium perfringens sepsis may produce a severe episode of acute hemolysis, with virtual opacity of the patient’s plasma due to hemoglobin released by the brisk intravascular hemolysis.
I. Hemoglobinopathies and Thalassemias
These extremely important conditions are covered in the final section. It should be noted that not all hemoglobinopathies or thalassemias produce hemolysis, but in some of them, especially sickle cell anemia and hemoglobin C disease, hemolysis dominates the clinical presentation.